Evaluation of the Oral Toxicity of Litchi Chinensis Pericarp Extract in Experimental Rats
Mayur Porwal1 , Phool Chandra1
, Phool Chandra1 , Vivek Kumar2
, Vivek Kumar2 , Navneet Verma3
, Navneet Verma3 and Km. Monika3*
and Km. Monika3*
1Teerthanker Mahaveer College of Pharmacy, Teerthanker Mahaveer University, Moradabad-244001, (U.P.), India.
2MET Faculty of Pharmacy, MIT Moradabad-244001, (U.P.), India.
3Pharmacy Academy, IFTM University, Lodhipur Rajput, Delhi Road (NH-24), Moradabad-244102, (U.P.), India.
Corresponding Author E-mail: iammonika1995@gmail.com
DOI : http://dx.doi.org/10.13005/ojc/390609
Article Received on : 07 Aug 2023
Article Accepted on :
Article Published : 18 Dec 2023
Reviewed by: Dr. M.A Shah
Second Review by: Dr. M.A Shah
Final Approval by: Dr. M.A Shah
A wide range of experiments have yielded empirical evidence pertaining to the efficacy of medicinal plants in the therapeutic treatment of several disorders. However, the use of herbs without conducting a thorough assessment of their effectiveness and safety can lead to sudden or harmful consequences that may pose a risk to the overall health of internal organs. Therefore, the current investigation’s goal was to determine the ethanolic extract of Litchi chinensis toxicological profile in rats. The Soxhlet extraction method extracted the fruit with ethanol as a solvent. The extract's susceptibility to acute, subacute, and subchronic toxicity was assessed. The histopathology of several organs (e.g., heart, liver, lungs, kidney and spleen) were also studied after treatment with plant extract. With the dosage of 2000 mg/kg, p.o., no deaths or adverse consequences were reported during the examination of acute toxicity. The Litchi chinensis extract produced no death or any observable changes in weight, behavior, organ weights, hematological or biochemical values in both oral subacute and subchronic toxicity experiments. Essential organs, including the heart, liver, lungs, kidney, and spleen, have regular planning when examined histopathologically, indicating no morphological changes. On the basis of results, the fruit (pericarp) extract of Litchi chinensis showed a lack of toxicity.
KEYWORDS:Acute Toxicit; Biochemistry; Hematology; Histopathology; Litchi Chinensis; Subacute Toxicity; Subchronic Toxicity
Download this article as:| Copy the following to cite this article: Porwal M, Chandra P, Kumar V, Verma N, Monika K. Evaluation of the Oral Toxicity of Litchi Chinensis Pericarp Extract in Experimental Rats. Orient J Chem 2023;39(6). |
| Copy the following to cite this URL: Porwal M, Chandra P, Kumar V, Verma N, Monika K. Evaluation of the Oral Toxicity of Litchi Chinensis Pericarp Extract in Experimental Rats. Orient J Chem 2023;39(6). Available from: https://bit.ly/3RuZ9Y5 |
Introduction
Herbal remedies have been employed for a wide range of medical conditions since antiquity. 1-4 . The utilization of flora is motivated by various factors, including commonplace, traditional, philosophical, and economic considerations, among others 5-8. Based on the World Health Organization’s findings, it has been observed that a significant proportion, approximately 80%, of the global population relies on medicinal plants for addressing their health-related needs 1, 7, 9. The utility, user-friendliness, and cost, as well as the mitigation of negative impacts, would contribute to this situation5, 6, 9. The medicinal properties of plants play a crucial role in the field of medical innovation, and their investigation serves as a viable approach for the exploration of novel pharmaceutical compounds 2, 10. Numerous experiments have provided empirical evidence regarding the effectiveness of herbal remedies in the therapeutic management of various ailments5, 9-11 .During the 19th and 20th centuries, there was a prevailing trend of toxicological revisionism. However, it is worth noting that toxicity is no longer considered a valid foundation for an alternative ethnopharmacological approach. This shift is due to the fact that regular individuals are now guided by conventional practices that prioritize global awareness and the selection of appealing species. From this standpoint, the assessment of toxicity is not primarily prioritized as the majority of well-informed botanical extracts are not deemed dangerous2. Plants produce a diverse array of metabolites, which manifest as complex compounds that can potentially have beneficial or harmful effects on human beings 10, 11. Nevertheless, despite the therapeutic potential of plants, several compounds derived from them have been unequivocally demonstrated to possess poisonous, teratogenic, and carcinogenic properties1, 9, 10. Despite the favorable attitudes expressed by patients towards their satisfaction with the use of herbal remedies and the therapeutic results obtained, as well as their dissatisfaction with the efficacy and safety of conventional allopathic or orthodox medicines, the issue of safety pertaining to herbal remedies remains a significant area of apprehension2, 9, 10. The investigations have received approval for the examination of over 150,000 plant species, revealing that a significant portion of these plants contain harmful substances 6. Moreover, it is widely recognized that the utilization of herbs without prior evaluation of their efficacy and safety may result in abrupt or toxic outcomes that could potentially harm the structural integrity of bodily organs10, 12. The findings of our current study indicate that the ethanolic extract of Litchi chinensis, referred to as EELC, exhibits promising in vivo anti-hyperlipidemic properties. In order to establish the anti-hyperlipidemic action, it is necessary to conduct toxicological examinations. In the pursuit of a pharmacological effect, it is customary to prioritize the assessment of toxicity and the determination of the lethal dose (LD50) associated with a drug 13. A valuable approach for narrowing down the investigation of pharmacological effects is the utilization of a toxicity study 9, 13.The statement posits that all substances possess poisonous properties, but their toxicity is contingent upon the quantity consumed. Exercising caution when handling medication is a direct consequence of the widely recognized Paracelsian principle. The issue of dose often presents a challenge due to the blurred distinction between therapeutic effects and harmful effects of drug14. Although Litchi chinensis is frequently employed in traditional medicine, there is a dearth of scientific evidence regarding its potential adverse effects 15. In order to mitigate this occurrence and ensure the safety of Litchi chinensis.
This research set out to answer some questions about the safety of Litchi chinensis by concentrating on the oral acute toxicity, subacute toxicity after 28 days, and subchronic toxicity after 90 days of administration to Wistar albino rats.
Materials and Methods
Chemical and Reagents
From Biolabs S.A. (Paris, France), we obtained commercially available reagent kits for the measurement of creatinine (CRE), urea (UR), glucose (GLU), total protein (TP), albumin (Alb), calcium (Ca2+), phosphorus (P), total cholesterol (TC), triglycerides (TG), aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), and Gamma glutamyl transferase (γ-GT). The best analytical chemicals and reagents were utilized, all of which were bought from commercial sources.
Plant Authentication
An expert botanist taxonomically identified, examined, and verified the Litchi chinensis plant fruit material. Plant authentication is carried out by Dr. Ashok Kumar, Botanist at IFTM University in Moradabad (U.P.), India. 2017/SOS/BOT/49 is the reference number. The fruit collection was finished in June at Mahakaleshwar Dham on NH-24, Delhi Road, in front of the Holiday Regency Hotel in Moradabad, India. For around 20 days, the fruits that had been gathered had dried up in the shade at ambient temperature.
Preparation of extraction
The powdered Litchi chinensis dried fruit material was run through a 20-mesh screen. With the use of a Soxhlet apparatus, 150 g of the fruit powder (Litchi chinensis) was defatted using petroleum ether (40–60) and then extracted with ethanol (95% v/v) for roughly 48 hours. After distilling the solvent from the plant’s extract of the fruits (Litchi chinensis), vacuum evaporator was used to filter and dry the extract. The plant’s (Litchi chinensis) ethanolic extract had a yield of 21.68%.
Experimental animals
In the current investigation, Wistar albino rats between 150 and 200g in body weight of either sex were employed. The IFTM University in Moradabad has an accredited animal home where the study’s test animals were kept. Animals were purchased from IFTM University’s animal house. The animals were kept in an equal day-night cycle that mimics nature. Comparatively, the temperature and relative humidity in the animal room were around 22°C (± 3oC) and 50–60%, respectively, while they had unlimited access to rodent standard food pellets and water. Before beginning an experimental behavioural investigation, animals were given four weeks to adapt. The test was carried out in an appropriate setting between 10:00 and 17:00. Every experimental methodology utilized in the research was approved via the Institutional Animals Ethics Committee (IAEC), IFTM University, Moradabad, affiliated with the Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA) (Ref. No.: 2017/837ac/MPH/13).
Acute oral toxicity
Healthy Wistar albino rats were used in accordance with the guidelines of The Organization for Economic Cooperation And Development (OECD) Guideline 42316 for testing of acute oral toxicity17, 18. Before the plant extract was administered, all animals were weighed, provided unlimited access to water, and fasted all night.
The animals has been randomly separated (total of 6 animals, 3 per group) into two groups based on their sex. Group 1 (Control) received ingestions of distilled water (1mL/100g), and Group 2 labeled “Acute toxicity was given a Litchi chinensis extract of 2000 mg/kg orally. After that, the animals are checked for any suspicious observations, like- mortality, acute toxicity, and behavioral abnormalities (agitation, drowsiness, odd vocalization), somnolence, tremors, convulsions, catatonia, fasciculation, paralysis, physical exhaustion, and abnormal motility and hypoxia). All of the test animals were kept apart and monitored daily for joint activity, body weight, severe symptoms, and mortality for the next 14 days. At the conclusion of the experiment, all animals were evaluated for weight, killed via cervical dislocation, and dissected for histopathology.
Subacute oral toxicity
According to OECD guideline 407, the test compounds are given orally daily to different groups of the research animals in progressive dosages, one dose level per group, for 28 days. The animals were attentively watched every day during the medication administration period to look for any signs of toxicity. Over the course of the research, each animal that passes away or is killed is necropsied. At the conclusion of the test, any remaining animals are likewise killed and necropsied. Upon reaching the termination of the examination, any surviving animals are euthanized and subjected to necropsy procedures. The animals were separated into two distinct groups for the purpose of conducting the studies (n=10 animals per group, 5 male and 5 females). The various dosages of EELC (400 mg/kg p.o. and 800 mg/kg p.o.) were chosen and delivered to each group by oral gavage daily for 28 days straight based on the acute oral toxicity research. The control group was administered solely with the vehicle (sterile water). Another group (Satellite) got the full 1000 mg/kg, p.o. dosage of EELC planned for 28 days while going untreated for an additional 14 days. For the analysis of reversibility, a satellite group must be applied. While administering the test chemical, it is crucial to utilize a satellite group to monitor the reversibility, determination, or delayed incidence of harmful qualities. The dosages were chosen in accordance with OECD Directive 407 19. After the Hippocratic screening, daily body weight, food and drink consumption, and the likely toxicity mark were set and documented. Every day, the clinical assessment passed.
Subchronic oral toxicity study
In albino Wistar rats, a 90-day oral toxicity study with repeated doses of EELC (Ethanolic Extract of Litchi chinensis) was conducted as per the OECD guidelines no. 40820. The test substance (Litchi chinensis) to rats was given varying doses of medication daily for a total of 90 days, and any symptoms of toxicity were monitored. The animals’ hematological and biochemical characteristics were observed. Ten rats—five female and five males—were divided into the control and treatment groups at random from a total of 20 rats. Rats in the two treatment groups received an aqueous solution of EELC by gavage at doses of 250 mg/kg PO per day and 1000 mg/kg PO per day, respectively, for a period of 90 days.
The dose of the test drug (Litchi chinensis) was selected based on acute toxicity study results. Control group animals received distilled water and a 90-day typical laboratory diet. The animals were pragmatic and rigorously intended for signs of any form of toxicity at the time of the study during the EELC delivery period. The cage-side behavior remarks of the experimental animals, such as food, water intake, body weight, and urine analysis, were carried out as part of the routine examination of the experimental animals to look for any changes. At the conclusion of the 90 days of the experimental study, the overnight fasting experimental animals were sacrificed using physical euthanasia (cervical dislocation, staining, etc.) techniques.
Clinical observations
A complete scientific assessment was performed on every experimental animal at least once before the first exposure and once a week after that. Whenever feasible, daily clinical inspections were made at least once per day at the precise times each day, considering the time of anticipated maximum effect following dosing. At least twice-daily checks and observations were made of all the experimental animals to note any signs of illness or death. Variations in the dermal, optical, mucous membranes, fur, frequency of secretion and excretion, and motor function during the research were among the signs of toxicity, but they weren’t the only ones (e.g., irregular breathing rhythm, lacrimation, large pupils, and piloerection).
Deviations in posture, gait, return to handling of the experimental animal, incidence of clonic or tonic activities, stereotypes (such as excessive grooming, repetitive circling), or sensory reaction to stimuli (such as walking backward, visual, and auditory), and odd behavior were noted. During the research period, each experimental animal was meticulously weighed at least once per week. At regular intervals of at least every week during the study, assessments of the water and food consumption of the test animals were made.
Hematology and clinical biochemistry
Hematological and biochemical blood samples were taken near the end of the testing period. By cardiac puncture and the retro-orbital method, blood samples were obtained and placed in ethylenediaminotetraacetic acid (EDTA) tubes. The blood samples of the experimental animals were analyzed. As the test period came to an end and any interim blood samples may have been taken, the following hematological and clinical chemistry tests were conducted.
Hematological investigations
Hematological testing was performed on blood that had been drawn into EDTA tubes. The parameters, such as (RBCs, WBCs, platelets, MCH, RDW, MCHC, PCV, etc.) were analyzed to check for any abnormalities. All these parameters were estimated at Diagno health care, Moradabad (U.P.)
Clinical biochemistry investigations
The biochemical parameters like sodium, potassium, glucose, urea, total cholesterol, creatinine, blood urea nitrogen, total protein, albumin, alkaline phosphate (ALP), Alanine aminotransferase, Aspartate aminotransferase, etc. were analyzed to check for any abnormalities. All these parameters were estimated at Diagno Health Care, Moradabad (U.P.).
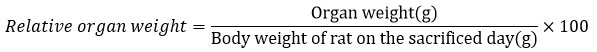
Relative organ weight
Qualitative information on the weight of various organs of the investigational animal, including the kidney, spleen, lungs, liver, and heart, was evaluated. Each organ of the animal used for the histopathology was suspiciously dissected from the sacrificed animals in addition to being them within a petri dish that contains 10% normal saline solution. The selected organs of the tested animal were dried using cotton wool and assessed by weighing it on a scale.
The weight of each organ of the test animal was standardized to the 100 g body weight of each rat using the formula shown below-
Histopathology
Gross necropsy was performed on all test animals utilized in the toxicity study. All significant pathological changes in major organs like- liver, spleen kidney, heart, and lungs were recorded for each animal. Microscopic assessment of organs of tested animals revealed that the proof of gross pathology inside the tested animals surviving 28 days after the initial dosing was measured may give up helpful data.
Statistical analysis
A two-way analysis of variance (ANOVA) was employed to examine variations among hematological parameters, body and organ weights, and water and food consumption, as well as between treated and control rats. The Bonferroni method was then utilized to determine the presence of significant differences. A significance level of 0.05 or lower (p<0.05) was deemed to be statistically significant. All the data were expressed as mean +- standard error of the mean (SEM). All of the analysis was done with the help of the statistical software – GraphPad PRISM (5.0)
Results
Acute oral toxicity
Neither mortality nor any symptoms of behavioral alterations were seen throughout the 14 days following an oral treatment of EELC up to the dosage of 2000 mg/kg, p.o. The morphological traits, such as fur, skin, eyes, and nose, are commonly observed. The patient’s posture and stride, reaction to handling and sensory inputs, and strength in the grip were all normal; there were no observed instances of tremors, convulsions, diarrhea, salivation, lethargy, or other strange behaviors were noticed. There was no significant difference between the control and treatment groups in terms of body weight or relative organ weight (Table 1) and (Table 2).
Table 1: Impact of EELC fruits on rat body weight over time (g).
|
Groups |
Body weight of rat (g) |
||
|
1st day |
7th day |
14th day |
|
|
Vehicle control |
118.00±1.15 |
122.00±1.00 |
124.00±1.20 |
|
2000mg/kg, p.o. EELC |
160.00±0.88*** |
175.00±0.88*** |
174±0.57*** |
EELC: Ethanolic extract of Litchi chinensis (2000 mg/kg). Data are represented as Mean ± SEM (n=3) for each group). P< 0.05 using Two-way analysis of variance with a Bonferroni post-test; ns: Not significant; * mild significant; ** moderate significant (P<0.01) and *** highly significant (P<0.001)
Table 2: Rats given a single dosage of EELC for 14 days and their relative organ weights
|
Organ |
Control |
EELC (2000 mg/kg, p.o.) |
|
Heart |
0.44±0.05 |
0.44±0.17ns |
|
Liver |
3.40±0.41 |
3.69±1.39 ns |
|
Kidney |
0.78±0.09 |
0.79±0.30 ns |
|
Spleen |
0.20±0.03 |
0.24±0.09 ns |
|
Lungs |
0.49±0.06 |
0.52±0.20 ns |
EELC: Ethanolic extract of Litchi chinensis (2000 mg/kg, p.o). Data are represented as Mean ± SEM (n=3) for each group. P< 0.05 using Two-way analysis of variance with a Bonferroni post-test; ns: Not significant; * mild significant; ** moderate significant (P<0.01) and *** highly significant (P<0.001).
The current investigation found no statistically significant differences between the EELC-treated group and the control group on hematological and biochemical indices (Table 3 and Table 4). There were no discernible changes between the various organs’ histological assessments stained with hematoxylin and eosin. (Fig. 1.). Hence, the LD50 of the extract was calculated to be more than 2000mg/kg, p.o.
Table 3: Effect of EELC on hematological markers in the acute toxicity investigation
|
Parameters |
Unit |
Control |
EELC (2000mg/kg, p.o.) |
|
Hemoglobin (Hb) |
g/L |
148.00±1.00 |
151.00±3.00 ns |
|
RBC Count |
1012/L |
8.49±0.19 |
9.3.00±0.16 ns |
|
Total Leukocyte Count (TLC) |
109/L |
4.30±0.10 |
9.20±0.10 ns |
|
Neutrophil |
% |
10.00±2.00 |
20.00±1.00 ns |
|
Lymphocyte |
% |
88.00±1.50 |
76.00±1.50* |
|
Eosinophil |
% |
1.00±0.50 |
2.00±0.50 ns |
|
Monocyte |
% |
1.00±0.50 |
2.00±0.50 ns |
|
Basophil |
% |
0.00±0.00 |
0.00±0.00 ns |
|
PCV/ Haematocrit |
L/L |
0.54±0.03 |
0.60±0.05 ns |
|
MCV |
Fl |
64.30±0.35 |
64.50±1.10 ns |
|
MCH |
Picogram |
17.40±0.65 |
16.20±0.90 ns |
|
MCHC |
g/L |
271.00±2.00 |
252.00±2.00*** |
|
Platelet Count |
109/L |
911.00±9.50 |
927.00±4.5*** |
|
RDW |
% |
13.10±0.15 |
19.40±0.70 ns |
|
ESR (Westegren’s Method) |
mm/1st hr |
8.00±0.50 |
10.00±0.50 ns |
EELC: Ethanolic extract of Litchi chinensis. Data are represented as Mean ± SEM; (n=3) for each group using Two-way analysis of variance with a Bonferroni post-test; ns: Not significant; * mild significant; ** moderate significant (P<0.01) and *** highly significant (P<0.001).
Table 4: Effects of EELC on biochemical markers in the acute toxicity investigation
|
Parameters |
Unit |
Control |
EELC (2000mg/kg,p.o.) |
|
Blood Urea |
mmol/L |
1.07±0.03 |
0.76±0.12 ns |
|
Serum Creatinine |
µmol/L |
15.90±0.55 |
17.10±0.40 ns |
|
Serum Uric Acid |
µmol/L |
76.90±1.55 |
66.70±1.15** |
|
Total Protein |
g/L |
69.00±1.50 |
69.00±2.00 ns |
|
Albumin |
g/L |
35.00±2.00 |
35.00±0.50 ns |
|
Globulin |
g/L |
34.00±1.50 |
34.00±0.50 ns |
|
A/G Ratio |
1.00±0.10 |
1.00±0.05 ns |
|
|
Sodium |
mmol/L |
137.00±1.00 |
139.00±2.50 ns |
|
Potassium |
mmol/L |
3.60±0.10 |
3.80±0.30 ns |
|
Calcium |
mmol/L |
2.20±0.20 |
2.19±0.05 ns |
|
Bilirubin (Total) |
µmol/L |
15.30±0.85 |
16.7±1.10 ns |
|
Conjugated (D. Bilirubin) |
µmol/L |
4.20±0.15 |
4.20±0.20 ns |
|
Unconjugated (I.D Bilirubin) |
µmol/L |
11.11±0.80 |
12.4±0.30 ns |
|
AST |
IU/L |
35.00±1.00 |
41.00±0.50 ns |
|
ALT |
IU/L |
39.00±1.00 |
44.00±2.00 ns |
|
Alkaline Phosphatase (ALP) |
IU/L |
579.00±5.00 |
294.00±2.50*** |
Data are represented as Mean ± SEM; (n=3) for each group). P< 0.05 Two-way analysis of variance with a Bonferroni post-test; ns: Not significant; * mild significant;** moderate significant (P<0.01) and *** highly significant (P<0.001).
 |
Figure 1: Histopathology of various organs in acute toxicity investigation. Heart, kidney, liver, spleen, and lungs of the control group are represented by letters A through E. |
A: Normal myocardium with muscle fibers (double arrow), Intercalated disc (up-arrow), nucleus (right arrow) and blood vessels (bent arrow). (H&E 20x); B: Liver of control rat; normal portal triads (up arrow) with normal hepatocytes. (H&E 20x); C: Kidney [collecting duct (arrow); DCT (up-arrow); Bowman’s space (down arrow); podocytes (elbow arrow connector). (H&E 40x); D: Spleen of control rat with normal histology; white pulp (arrow), the red pulp (elbow arrow), central artery (right arrow). (H&E 20x); E: Normal Lungs of control rat. (H&E 20x); F: Heart of rat in acute toxicity normal myocardium. (H&E 20x); G: Liver of rat in acute toxicity; mild congestion at portal vein (down arrow) with normal surrounding hepatocytes. (H&E 20x); H: Kidney of rat in acute toxicity; normal tubules (arrow) with some intertubular capillary congestion (up-arrow). (H&E 40x); I: Spleen of rat in acute toxicity with minimal occlusion in the red pulp (arrow). (H&E 20x); J: Lungs of rat in acute toxicity with normal histology. (H&E 20x)
Subacute oral toxicity
Weekly body weight
Group I consist of EELC of 400mg/kg, and group II EELC consists of 800mg/kg. The three groups determined weekly body weight on the initial (0) days, 7th, 14th, 21th, and 28th days. The bodyweight of rats in control (118±1.15) as well as in other extract groups I (166±0.33) and II (144±1.45) showed a gradual increase during the study (Table 5).
Table 5: Time course of the effect of EELC on body weight (g) in rats
|
Group |
Dose |
Weight (g) |
||||
|
Initial day |
7th day |
14th day |
21st day |
28th day |
||
|
Control |
3ml/kg |
118.00±1.15 |
122.00±1.00 |
124.00±1.20 |
126.00±1.20 |
128.00±1.76 |
|
I |
400mg/kg |
155.00±0.88*** |
156.00±0.88 *** |
162.00±1.76*** |
164.00±0.57*** |
166.00±0.33*** |
|
II |
800mg/kg |
126.00±1.00ns |
132.00±1.15*** |
135.00±1.45*** |
142.00±2.08*** |
144.00±1.45*** |
Groups I-II: Ethanolic extract with doses (I: 400 mg/kg; II: 800 mg/kg); Data are represented as Mean ± SEM (n=10; for each group 5 male, 5 female); P< 0.05 Two-way analysis of variance with a Bonferroni post-test; ns: Not significant; * mild significant; ** moderate significant (P<0.01) and *** highly significant (P<0.001).
Observation and mortality
No negative side effects were observed in rats when EELC was given orally once a day for 28 days, even at the maximum dose tested (800 mg/kg, p.o. body weight). There were no changes between the animals’ health and that of the control group. There were no appreciable weight differences between the treatment and control groups, and there was no mortality noted during the investigation.
Relative organ weight
There was no statistically significant difference between the treatment groups and the control group in terms of the absolute weights of the organs as stated at necropsy (P > 0.05) (Table 6).
Table 6: Rats given varying dosages of EELC treatment for 28 days and their relative organ weights.
|
Group |
Treatment |
Dose |
Liver (g) |
Kidney (g) |
Spleen (g) |
|
Control |
Distilled water |
3ml/kg |
3.40± 0.41 |
0.78±0.09 |
0.20±0.03 |
|
I |
EELC Low Dose |
400mg/kg |
2.77±0.92ns |
0.68±0.22 ns |
0.24±0.08 ns |
|
II |
EELC High Dose |
800mg/kg |
3.40±0.88 ns |
0.77±0.20 ns |
0.26±0.06 ns |
EELC: I-II Ethanolic extract of Litchi chinensis with doses (I: 400 mg/kg and II: 800 mg/kg). Data are represented as Mean ± SEM (n=10; 5 males and 5 females) using Two-way analysis of variance with a Bonferroni post-test; ns: Not significant; * mild significant; ** moderate significant (P<0.01) and *** highly significant (p<0.001).
Hematological parameters
The impact of repeated oral EELC dosages on hematological markers is described in (Table 7). The hematological test could not identify any significant variations between the therapy and a control group. Apart for modest differences in a few parameters, the majority of hematological measurements in treated rats, including hemoglobin, total red blood cell count, red cell distribution width, erythrocyte sedimentation rate, white blood cell count, neutrophil count, lymphocyte count, monocyte count, and platelet count did not exhibit significant variations compared to the control group.
Table 7: Effect of EELC on hematological markers in subacute toxicity investigation.
|
Parameters |
Unit |
Control |
EELC (800mg/kg, p.o.) |
|
Hemoglobin (Hb) |
g/L |
148.00±1.00 |
139±2.00 ns |
|
RBC Count |
1012/L |
8.49±0.19 |
8.56±0.27 ns |
|
Total Leucocyte Count (TLC) |
109/L |
4.30±0.10 |
7.4±0.40 ns |
|
Neutrophils |
% |
10.00±2.00 |
12±1.50 ns |
|
Lymphocyte |
% |
88.00±1.50 |
84±3.00 ns |
|
Eosinophils |
% |
1.00±0.50 |
02±0.50 ns |
|
Monocyte |
% |
1.00±0.50 |
02±0.50 ns |
|
Basophil |
% |
0.00±0.00 |
0.00±0.00 ns |
|
PCV/ Haematocrit |
L/L |
0.54±0.03 |
0.51±0.01 ns |
|
MCV |
Fl |
64.3±0.35 |
60.40±0.80 ns |
|
MCH |
Picogram |
17.40±0.65 |
16.20±0.45 ns |
|
MCHC |
g/L |
271.00±2.00 |
269.00±1.50 ns |
|
Platelet Count |
109/L |
911.00±9.50 |
865.00±7.50*** |
|
RDW |
% |
13.10±0.15 |
14.60±0.55 ns |
|
ESR (Westegren’s Method) |
mm/1st hr |
8.00±0.50 |
35.00±1.50*** |
Data are represented as Mean ± SEM (n=10; for each group) using Two-way analysis of variance with a Bonferroni post-test; ns: Not significant; * mild significant; ** moderate significant (P<0.01) and *** highly significant (P<0.001).
Biochemical analysis
Table 8 shows the impact of repeated doses of EELC taken orally on serum toxicity indicators such AST, ALT, and ALP. Findings demonstrated that there were no appreciable differences between treated and control animals’ values. The serum electrolytes (Na+, K+, and Cl-) were unaffected by the EELC. Urea, uric acid and creatinine levels, which are markers of renal function, did not show any appreciable changes. Apart for minor fluctuations, there were no statistically noteworthy alterations in the liver function measures (AST, ALT, and ALP). Moreover, there were no discernible increases in total protein, albumin, or globulin. (Table 8).
Table 8: Subacute toxicity investigation of EELC on biochemical markers
|
Parameters |
Unit |
Control |
EELC (800mg/kg, p.o.) |
|
Blood Urea |
mmol/L |
1.07±0.03 |
0.95±0.04 ns |
|
Serum creatinine |
µmol/L |
15.90±0.55 |
20.60±0.80 ns. |
|
Serum uric acid |
µmol/L |
76.90±1.55 |
87.20±1.10 ns |
|
Total protein |
g/L |
69.00±1.50 |
68.00±1.00 ns |
|
Albumin |
g/L |
35.00±2.00 |
39.00±0.50 ns |
|
Globulin |
g/L |
34.00±1.50 |
29.00±1.00 ns |
|
A/G Ration |
– |
1.00±0.10 |
1.30±0.05 ns |
|
Sodium |
mmol/L |
137.00±1.00 |
135.00±1.50 ns |
|
Potassium |
mmol/L |
3.60±0.10 |
4.00±0.25 ns |
|
Calcium |
mmol/L |
2.20±0.20 |
2.47±0.16 ns |
|
Bilirubin (Total) |
µmol/L |
15.30±0.85 |
16.41±0.69 ns |
|
Conjugated (Direct bilirubin) |
µmol/L |
4.20±0.15 |
4.40±0.20 ns |
|
Unconjugated (Indirect Bilirubin) |
µmol/L |
11.11±0.80 |
11.90±0.15 ns |
|
Total Protein |
g/L |
69.00±1.50 |
68.00±1.00 ns |
|
Albumin |
g/L |
35.00±2.00 |
39.00±0.50 ns |
|
Globulin |
g/L |
34.00±1.50 |
29.00±1.00 ns |
|
A/G Ratio |
|
1.00±0.10 |
1.30±0.05 ns |
|
AST |
IU/L |
35.00±1.00 |
44.00±2.50*** |
|
ALT |
IU/L |
39±1.00 |
38.00±1.00 ns |
|
Alkaline Phosphatase (ALP) |
IU/L |
579.00±5.00 |
254.00±3.00*** |
Data are represented as Mean ± SEM (n=10; for each group). ); P< 0.05 using Two-way analysis of variance with a Bonferroni post-test; ns: Not significant; * mild significant; ** moderate significant (P<0.01) and *** highly significant (P<0.001).
Histopathology
Several organs, including the liver, heart, spleen, lung, and kidney, were examined under the microscope and found to be structurally normal and free of overt pathological abnormalities in both the control and treatment groups (Fig. 2.).
 |
Figure 2: Several organs were examined histopathologically in a study of subacute oral toxicity. |
K: Liver of control rat; normal portal triads (up arrow) with normal hepatocytes. (H&E 20x); L: Kidney [collecting duct (arrow); DCT (up-arrow); Bowman’s space (down arrow); podocytes (elbow arrow connector). (H&E 40x); M: Spleen of control rat with normal histology; white pulp (arrow), the red pulp (elbow arrow), central artery (right arrow). (H&E 20x); N: Liver of rat in subacute toxicity; mild dilatation and congestion in the portal vein (right arrow). (H&E 20x); O: Kidney of rat in subacute toxicity; alterations in convoluted tubules characterized by hypertrophy (arrow), Expansion of tubules (up-down arrow) and necrosis (double arrow). (H&E 40x); P: Spleen of rat in subacute toxicity having moderate congestion of red pulp with a large number of RBCs (arrow). (H&E 40x).
Subchronic oral toxicity
Weekly body weight
The first one is control one, Group I consist of EELC of 250mg/kg and II group EELC of 1000mg/kg, p.o. The four groups determined weekly body weight on the initial (0) day, 15th, 30th, 45th, 60th and 90th days. The bodyweight of rats in control (115±1.66) as well as in other extract groups I (127±0.88) and II (142±1.15) showed a gradual increase during the study (Table 9).
Table 9: Effects of the pericarp of EELC fruits on the body weights of rats (g) on various days.
|
Group |
Dose |
Weight (g) |
||||||
|
Initial day |
15th day |
30th day |
45th day |
60th day |
75th Day |
90th day |
||
|
Control |
3ml/kg |
115.00±1.66 |
117.00±1.52 |
119.00±1.52 |
120.00±1.85 |
122.00±1.85 |
123.00±1.85 |
124.00±1.85 |
|
I |
250mg/kg |
127.00±0.88** |
130.00±0.88*** |
133.00±0.57*** |
135.00±0.88*** |
140.00±0.33*** |
142.00±0.88*** |
144.00±0.33*** |
|
II |
1000mg/kg |
142.00±1.15*** |
145.00±1.20*** |
152.00±1.76*** |
178.00±3.51*** |
187.00±3.51*** |
191.00±3.05*** |
193.00±1.66*** |
Groups I-II Ethanolic extract with doses (I: 250 mg/kg and II: 100 mg/kg). Data are represented as Mean ± SEM (n=10; with male=5; female=5) using Two-way analysis of variance with a Bonferroni post-test. ns: not significant, * mild significant;** moderately significant (p<0.01) and *** highly significant (P<0.001).
Observations and mortality
The maximum dose studied, 1000 mg/kg, p.o. body weight, did not cause any toxic effects in rats when given orally daily for 90 days. There were no changes between the animals’ health and that of the group acting as control. The importance of the treated groups comparative to the control groups did not vary significantly, and no death was tracked throughout the experimental procedures.
Relative organs weight
When compared to the control, the organ weight compared to body weight of each individual organ reported at necropsy in the other groups did not change significantly (P > 0.05). (Table 10)
Table 10: the relative organ weight of rats given EELC treatments at various dosages for 90 days.
|
Group |
Liver (g) |
Kidney (g) |
Spleen (g) |
|
Control |
3.40± 0.41 ns |
0.78±0.09 ns |
0.20±0.03 ns |
|
I |
2.90±0.64ns |
0.65±0.15 ns |
0.21±0.73 ns |
|
II |
2.39±1.12 ns |
0.50±0.23 ns |
0.15±0.07 ns |
Groups I-II Ethanolic extract with doses (I: 250 mg/kg and II: 1000 mg/kg). Data are represented as Mean ± SEM (n=10; with male=5; female=5) using Two-way analysis of variance with a Bonferroni post-test. ns: not significant. Relative organ weight was computed with the help of (organ weight/body weight) ×100
Hematological parameters
Table 11 shows the impact of repeated doses of orally given EELC on hematological parameters. Hematological analysis failed to show any significant differences between the experimental groups and the controls. Apart for modest differences in a few specific parameters, the majority of hematological measurements in treated rats, including hemoglobin, total red blood cell count, red cell distribution width, erythrocyte sedimentation rate, white blood cell count, neutrophil count, lymphocyte count, monocyte count, and platelet count did not exhibit significant variations compared to the control group.
Table 11: Effect of EELC on hematological markers in the subchronic toxicity investigation.
|
Parameters |
Unit |
Control |
EELC (250mg/kg, p.o.) |
EELC (1000mg/kg, p.o.) |
|
Haemoglobin |
g/L |
148.00±1.00 |
132.00±1.50 ns |
150.00±1.50*** |
|
RBC Count |
1012/L |
8.49±0.19 |
7.18±0.16 ns |
9.03±0.11 ns |
|
Total Leucocytes Count |
109/L |
4.30±0.10 |
6.80±0.25 ns |
10.40±0.15 ns |
|
Neutrophil |
% |
10±2.00 |
70±1.00*** |
68±1.50*** |
|
Lymphocyte |
% |
88±1.50 |
28±1.50*** |
30±1.00*** |
|
Eosinophil |
% |
1.00±0.50 |
2.00±0.50 ns |
02±0.50 ns |
|
Monocyte |
% |
1.00±0.50 |
00±0.00 ns |
00±0.00 ns |
|
Basophil |
% |
1.00±0.50 |
00±0.00 ns |
00±0.00 ns |
|
HCT |
L/L |
0.54±0.03 |
0.43±0.05 ns |
0.5±0.03 ns |
|
MCH |
Pg |
17.40±0.65 |
18.50±0.70*** |
16.60±0.35*** |
|
MCV |
Fl |
64.30±0.35 |
60.40±0.80*** |
55.40±1.80*** |
|
MCHC |
g/L |
271.00±2.00 |
306.00±4.50*** |
300.00±4.0*** |
|
Platelet Count |
109/L |
911.00±9.50 |
652.00±3.00*** |
924.00±6.50*** |
Data are represented as Mean ± SEM (n=10; with male=5; female=5 for each group); P<0.001 using Two-way analysis of variance with a Bonferroni post-test; ns: Not significant, * mild significant; ** moderately significant (P<0.01) and *** highly significant (P<0.001).
Biochemical analysis
The impact of repeated oral EELC dosages on blood toxicity indicators (AST, ALT, and ALP, among others) is described in (Table 12). Findings demonstrated that there were no appreciable differences between treated and control animals’ values. The serum electrolytes (Na+, K+, and Cl-) were unaffected by the EELC. Urea, uric acid and creatinine levels, which are markers of renal function, did not show any appreciable changes. Apart for minor fluctuations, there were no statistically noteworthy differences in the liver function measures (SGOT, SGPT, and ALP). Moreover, there were no discernible increases in total protein, albumin, or globulin. (Table 12).
Table 12: Sub chronic toxicity investigation of EELC on biochemical markers.
|
Parameters |
Unit |
Control |
EELC (250mg/kg, p.o.) |
EELC (1000mg/kg, p.o.) |
|
Total Bilirubin |
µmol/L |
15.30±0.85 |
11.80±0.37 ns |
15.05±0.15 ns |
|
Direct Bilirubin |
µmol/L |
4.20±0.15 |
5.98±0.36 ns |
7.18±0.40 ns |
|
Indirect Bilirubin |
µmol/L |
11.11±0.80 |
5.81±0.12 ns |
7.86±0.14 ns |
|
Proteins |
g/L |
69.00±1.50 |
76.00±2.00 ns |
75.00±3.50 ns |
|
Albumin |
g/L |
35.00±2.00 |
50.00±2.00 ns |
42.00±1.00** |
|
AST |
IU/L |
35.00±1.00 |
49.00±2.50*** |
152.00±0.95** |
|
ALT |
IU/L |
39.00±1.00 |
61.20±1.00*** |
180.2±1.90*** |
|
ALP |
IU/L |
579.00±5.00 |
109.70±4.50*** |
99.00±4.15*** |
|
Blood Urea |
mmol/L |
1.07±0.03 |
0.37±0.17 ns |
1.06±0.01 ns |
|
Serum Creatinine |
µmol/L |
15.90±0.55 |
14.02±0.09 ns |
18.81±0.99 ns |
Data are represented as Mean ± SEM (n=10; with male=5; female=5); P<0.001 Two-way analysis of variance with a Bonferroni post-test; ns: Not significant, * mild significant; ** moderately significant (P<0.01) and *** highly significant (P<0.001).
Histopathology
In both the control and treatment groups, microscopic analysis of sections from several organs such the kidney, liver, heart, spleen, and lungs revealed normal histology and a lack of any obvious pathological abnormalities (Fig. 3).
 |
Figure 3: Histopathological study of various organs in subchronic oral toxicity study. Liver, Kidney, and Spleen are represented by Q, R, and S in the Control group. |
Q: Liver of control rat; normal portal triads (up arrow) with normal hepatocytes. (H&E 20x); R: Kidney [collecting duct (arrow); DCT (up-arrow); Bowman’s space (down arrow); podocytes (elbow arrow connector). (H&E 40x); S: Spleen of control rat with normal histology; white pulp (arrow), the red pulp (elbow arrow), central artery (right arrow). (H&E 20x); T: Liver of rat in sub chronic toxicity; mild dilatation (curved up-arrow) and congestion (up-arrow) in a central vein. (H&E 20x); U: Kidney of rat in subchronic toxicity; mild congestion (right arrow) and normal tubules. (H&E 40x); V: Spleen of rat in sub chronic toxicity with moderate congestion of red pulp (arrow) followed by necrosis (right arrow). (H&E 40x).
Discussion
Conventionally, the corresponding drug has been utilized for centuries. It is an evidence-based remedy with its attractiveness and well-known utilization1, 21. Defects in the legislation and precise procedures are rare and have harmful effects. This might be as a result of inadequate scientific research understanding and drug evaluation study methodologies1, 22. As a result, several plants and their mixtures have been identified as being toxic globally4, 23, 24 .The Food and Drug Administration has delivered forewarnings on the likely negative impact of a number of regularly used herbal treatments or herbal formulations1, 23 .Therapeutic plants utilized in different parts of the human race have been shown to carry toxicological concerns13 .To make herbal therapies more widely accepted, their market must first undergo safety studies before it can be standardized, regulated, or both1, 7. Preliminary to a few pharmacological validations and acute, subacute, and subchronic toxicity testing for any medicinal plant must be carried out in compliance with OECD regulations before the plant is developed into a phytomedicine13, 25. It is crucial for determining preclinical dosage during the drug research and development process13, 22. As a result, toxicity offers the correct order of potentially applicable adverse effects of the evaluated substance26. In order to generate evidence that meets the requirements needed to justify traditional medicines’ widespread usage, scientists have recently explored the health benefits and efficacy potential of these treatments1, 10, 27. Historically, the medicinal herb Litchi chinensis has been used to treat and manage a wide range of ailments, but no systematic data is to be handed thus on its safety. From a pharmacological angle, the present plant is among those utilized as an anti-inflammatory, antioxidant, and antibacterial agent.28 In a recent study, Wistar rats were used to assess the acute, subacute, and subchronic toxicity tests of the physical, biochemical, hematological, and histopathological critical organs, as well as the protective effects of the fruit extract of Litchi chinensis. One single dose of 2000 mg/kg, p.o. was used in the acute toxicology research, of the fruit extract from Litchi chinensis did not result in any deaths, clinical signs of increased or decreased body temperature, variations in the color of the skin or eyes, generalized ill-appearance, diarrhea, or drowsiness. In light of this, the fruit extract’s LD50 is greater than 2000 mg/kg. Compared to the control group, the EELC 2000 mg/kg, p.o. has a significantly effective effect on MCH and platelet count in the hematological parameter. In biochemical parameters, the EELC (2000 mg/kg, p.o.) produces a moderately significant effect on serum uric acid, decreases the serum uric acid, and produces a highly effective impact on alkaline phosphatase (ALP) with a reduced level of ALP. Decreased level of ALP causes hypophosphatasia an atypical genetic disorder that affects bones and teeth. Two dosages i.e., 400 and 800mg/kg/day, p.o. of plant extract were used in the subacute toxicity trial over the course of 28 days.
The bodyweight of the rats in the control group (118±1.15), group I (155±0.88), and group II (126±1.00), all gradually increased during the course of the research. The treated groups showed no signs of poisoning or death. When Litchi chinensis meal and water are taken orally for 28 days, intake is no longer impacted. It demonstrates that the extract had no negative impacts on animal growth or its ability to affect appetite. The liver of rats in subacute toxicity showed mild dilatation and congestion in the portal vein. Kidney of rats in subacute toxicity showed alterations in convoluted tubules characterized by hypertrophy (arrow), Expansion of tubules (up-down arrow), and necrosis.
The spleen of animals in the subacute toxicity study had moderate congestion of red pulp with a large number of RBCs (arrow) of Litchi chinensis in contrast to the normal control group. Our findings proposed that Litchi chinensis, at the uppermost dose, may cause edema in rats via boosting RBC production. Rats are typically a little more sensitive, therefore this shift in their RBCs was thought to be a little physiological difference since the values fell inside the defined range and were assumed to be accidental owing to the lack of dosage dependence29. Our therapeutic dosages, which were less than 2000 mg/kg at 400 and 800 mg/kg were employed. Two dosages of 250 and 1000 mg/kg, p.o./day were used to evaluate the subchronic toxicity research for a period of 90 days. The first is the control, which consists of 250 mg/kg of p.o. EELC and II group has EELC of 1000mg/kg, p.o. Rats in the extract groups I and II (127± 0.88% and 142 ±1.15%, respectively) as well as the control group (115± 1.66) gradually gained weight during the course of the research. In the treated groups, there was no analysis for toxicity or mortality. Meal and water consumption were unaffected 90 days after the oral dose of Litchi chinensis. It showed that there was no effect on appetite from the extract. The liver of rats with subchronic toxicity presented a mild dilatation (curved up-arrow) and congestion (up-arrow) in the central vein. The rats with subchronic toxicity kidney showed mild congestion (right arrow) and normal tubules. The spleen of rats in subchronic toxicity with moderate congestion of red pulp (arrow) followed by necrosis (right arrow) of Litchi chinensis as a contrast to the normal control set. Our findings advocated that Litchi chinensis, at uppermost dose, may cause edema in rats via boosting RBC production. Due to the lack of dosage dependence, the change in RBCs seen in the rats was thus thought to be a small physiological difference; in general, they are somewhat more sensitive. They were also found to be within the normal range29. Rather than this, the EELC 100mg/kg produces a highly significant effect on hemoglobin, neutrophils, lymphocytes, MCH, MCV, MCHC, and platelet count. At 250 mg/kg, p.o. the EELC produces highly significant on neutrophils, lymphocytes, MCH, MCV, MCHC, and platelet count. On the biochemical parameter, the EELC 1000 mg/kg, p.o. produces a moderately significant effect on albumin and AST, whereas highly significant on ALT and ALP. The EELC 250 mg/kg, p.o. has a highly effective impact on ALT, AST, and ALP at what time contrast with control group animals.
It is crucial to understand the comprehensive state of these two essential vital organs in order to predict the toxicity of any new or novel molecule. This may be accomplished by doing a biochemical examination 3. Biomarkers for the kidney and liver show that the extract is safe at the studied level. The levels of total protein and albumin in both gender of rats did not change when Litchi chinensis was supplied at any dose. Similar to this, animal serum lipid measurements have not changed. These outcomes recommend that the Litchi chinensis extract may not have poisonous substances 30 which would somewhat elucidate its wellbeing.
Conclusion
There was no indication of toxicity or treatment-related mortality in rats following oral administration of an ethanolic extract of the fruit (pericarp) of Litchi chinensis at a dose of 2000 mg/kg p.o. Repeated dosages of 250-1000 mg/kg, p.o. for 90 days and repeated doses of 400 mg/kg up to 800 mg/kg, p.o. planned for 28 days did not significantly alter the amount of food and water consumed. No pronounced effects were also established in hematological, biochemical analyses, and histopathological stage. The risk-to-benefit proportion included in this analysis is in the favor of using this traditional herb.
The fruit (pericarp) extract of Litchi chinensis can thus be utilized due to its shown lack of toxicity, and because therapeutic dosages are far lower than LD50 and toxic levels, it may be used in the long-term treatment.
Acknowledgments
It’s my privilege to express my obligation and heartfelt gratitude to Vice-Chancellor, IFTM University, Moradabad (U.P.) India for his continuous encouragement and support in laboratories of the Faculty of Pharmacy.
Conflict of Interest
There is no conflict of interest
Funding Sources
No funding was received. Availability of the data and materials- All data and materials are available upon request.
References
- Kale, O. E.; Awodele, O., Akindele, A. J. Subacute and subchronic oral toxicity assessments of Acridocarpus smeathmannii (DC.) Guill. & Perr. root in Wistar rats. Toxicol Rep. 2019, 6, 161-175.
- Ahmad, L.; He, Y.; Hao, J. C.; Semotiuk, A.; Liu, Q. R., Mazari, P. Toxic pyrrolizidine alkaloids provide a warning sign to overuse of the ethnomedicine Arnebia benthamii. J Ethnopharmacol. 2018, 210, 88-94.
- Sureshkumar, D.; Begum, S.; Johannah, N. M.; Maliakel, B., Krishnakumar, I. M. Toxicological evaluation of a saponin-rich standardized extract of fenugreek seeds (FenuSMART(®)): Acute, sub-chronic and genotoxicity studies. Toxicol Rep. 2018, 5, 1060-1068.
- Agarwal, A.; Chakraborty, P.; Chakraborty, D. D., Saharan, V. A. Phytosomes: Complexation, Utilisation and Commerical Status. Journal of Biologically Active Products from Nature. 2012, 2 (2), 65-77.
- Upadhyay, P.; Purohit, S.; Mishra, S.; Tiwari, K.; Dubey, G., FARAG MR, S. H. J. I. J. G. P. Pharmacognostic standardization of Asian folk medicinal plant Reinwardtia Indica Dumort. Int J Green Pharm. 2018, 12 (2), S380-S385.
- Boukandou Mounanga, M.; Mewono, L., Aboughe Angone, S. Toxicity studies of medicinal plants used in sub-Saharan Africa. J Ethnopharmacol. 2015, 174, 618-627.
- Habbu, P.; Madagundi, S.; Kulkarni, R.; Jadav, S.; Vanakudri, R., Kulkarni, V. Preparation and evaluation of Bacopa–phospholipid complex for antiamnesic activity in rodents. Drug Invention Today. 2013, 5 (1), 13-21.
- Njan, A. A.; Olaoye, S. O.; Afolabi, S. O.; Ejimkonye, B. C.; Soje, A.; Olorundare, O. E., Iwalewa, E. O. Safety effect of fractions from methanolic leaf extract of Ocimum gratissimum on reproduction in male wistar rats. Toxicol Rep. 2019, 6, 496-504.
- Ugwah-Oguejiofor, C. J.; Okoli, C. O.; Ugwah, M. O.; Umaru, M. L.; Ogbulie, C. S.; Mshelia, H. E.; Umar, M., Njan, A. A. Acute and subacute toxicity of aqueous extract of aerial parts of Caralluma dalzielii N. E. Brown in mice and rats. Heliyon. 2019, 5 (1), e01179.
- Singh, R. P.; Gangadharappa, H. V., Mruthunjaya, K. Phospholipids: Unique carriers for drug delivery systems. Journal of Drug Delivery Science and Technology. 2017, 39, 166-179.
- Sani, T. A.; Mohammadpour, E.; Mohammadi, A.; Memariani, T.; Yazdi, M. V.; Rezaee, R.; Calina, D.; Docea, A. O.; Goumenou, M., Etemad, L. J. F. Cytotoxic and apoptogenic properties of Dracocephalum kotschyi aerial part different fractions on calu-6 and mehr-80 lung cancer cell lines. Farmacia. 2017, 65 (2), 189-199.
- Shaw, D. Toxicological risks of Chinese herbs. Planta Med. 2010, 76 (17), 2012-2018.
- Pare, D.; Hilou, A.; N’Do, J.; Guenne, S.; Sombie, E., Kpemissi, M. Protective effect of bioactive fractions of C. Dalzielii against weight gain in mice feed with high fat-diet. International Journal of Scientific Research. 2021, 10, 10.
- Kpemissi, M.; Metowogo, K.; Melila, M.; Veerapur, V. P.; Negru, M.; Taulescu, M.; Potârniche, A. V.; Suhas, D. S.; Puneeth, T. A.; Vijayakumar, S.; Eklu-Gadegbeku, K., Aklikokou, K. Acute and subchronic oral toxicity assessments of Combretum micranthum (Combretaceae) in Wistar rats. Toxicol Rep. 2020, 7, 162-168.
- Chukwuma, C. I.; Izu, G. O.; Chukwuma, M. S.; Samson, M. S.; Makhafola, T. J., Erukainure, O. L. A review on the medicinal potential, toxicology, and phytochemistry of litchi fruit peel and seed. Journal of Food Biochemistry. 2021, 45 (12), e13997.
- OECD. Test No. 423: Acute Oral toxicity – Acute Toxic Class Method2002.
- Procházková, D.; Boušová, I., Wilhelmová, N. Antioxidant and prooxidant properties of flavonoids. Fitoterapia. 2011, 82 (4), 513-523.
- Tchoumtchoua, J.; Mouchili, O. R.; Ateba, S. B.; Zingue, S.; Halabalaki, M.; Mbanya, J. C.; Skaltsounis, A. L., Njamen, D. Safety assessment of the methanol extract of the stem bark of Amphimas pterocarpoides Harms: Acute and subchronic oral toxicity studies in Wistar rats. Toxicol Rep. 2014, 1, 877-884.
- OECD. Test No. 407: Repeated Dose 28-day Oral Toxicity Study in Rodents2008.
- OECD. Test No. 408: Repeated Dose 90-Day Oral Toxicity Study in Rodents2018.
- Catarino, L.; Havik, P. J., Romeiras, M. M. Medicinal plants of Guinea-Bissau: Therapeutic applications, ethnic diversity and knowledge transfer. J Ethnopharmacol. 2016, 183, 71-94.
- Mazumder, A.; Dwivedi, A.; du Preez, J. L., du Plessis, J. In vitro wound healing and cytotoxic effects of sinigrin-phytosome complex. Int J Pharm. 2016, 498 (1-2), 283-293.
- De Smet, P. A. Health risks of herbal remedies: an update. Clin Pharmacol Ther. 2004, 76 (1), 1-17.
- Skalicka-Wozniak, K.; Georgiev, M. I., Orhan, I. E. Adulteration of herbal sexual enhancers and slimmers: The wish for better sexual well-being and perfect body can be risky. Food Chem Toxicol. 2017, 108 (Pt B), 355-364.
- El-Gazayerly, O. N.; Makhlouf, A. I.; Soelm, A. M., Mohmoud, M. A. Antioxidant and hepatoprotective effects of silymarin phytosomes compared to milk thistle extract in CCl4 induced hepatotoxicity in rats. J Microencapsul. 2014, 31 (1), 23-30.
- Jordan, S. A.; Cunningham, D. G., Marles, R. J. Assessment of herbal medicinal products: challenges, and opportunities to increase the knowledge base for safety assessment. Toxicol Appl Pharmacol. 2010, 243 (2), 198-216.
- Kale, O. E.; Oyesola, T. O., Raji, F. S. Celecoxib, a cyclooxygenase-2 inhibitor, offers chemoprevention against reproductive and neurobehavioural abnormalities induced by atrazine in male Wistar rats. Environ Toxicol Pharmacol. 2018, 58, 84-97.
- Kpemissi, M.; Eklu-Gadegbeku, K.; Veerapur, V. P.; Potârniche, A. V.; Adi, K.; Vijayakumar, S.; Banakar, S. M.; Thimmaiah, N. V.; Metowogo, K., Aklikokou, K. Antioxidant and nephroprotection activities of Combretum micranthum: A phytochemical, in-vitro and ex-vivo studies. Heliyon. 2019, 5 (3), e01365.
- Ateba, S. B.; Simo, R. V.; Mbanya, J. C.; Krenn, L., Njamen, D. Safety profile and gender specific differences of a methanol extract of Eriosema laurentii (Leguminosae) in acute and subchronic (28 days) oral toxicity studies in Wistar rats. Food Chem Toxicol. 2014, 65, 27-32.
- Ragavendran, P.; Sophia, D.; Arul Raj, C., Gopalakrishnan, V. Functional group analysis of various extracts of Aerva lanata (L.,) by FTIR spectrum. Pharmacologyonline. 2011, 1, 358-364.
Abbreviations
LC: Litchi chinensis; EELC: Ethanolic extract of Litchi chinensis; LD50: median lethal dose; WHO: World Health Organization; TG Triglycerides; CRE creatinine; UR urea; GLU glucose; TP Total protein; AST Aspartate aminotransferase; Alb albumin; ALT alanine aminotransferase; γ-GT Gamma-glutamyl transferase; CPCSEA Committee For The Purpose Of Experiment On Animal; IAEC Institutional Animal Ethics Committee; OECD Organization for Economic Cooperation and Development; Hb Hemoglobin; TLC Total leukocytes count; MCV Mean corpuscular volume; MCH Mean corpuscular hemoglobin; MCHC Mean corpuscular hemoglobin concentration; RDW Red blood cell distribution cell distribution width; ESR Erythrocyte sedimentation rate.

This work is licensed under a Creative Commons Attribution 4.0 International License.









